Probiotics are defined by the World Health Organization (WHO) as living microorganisms which, when administered in adequate amounts, confer a health benefit upon the host.
This refers to ‘live’ beneficial bacteria or the good bacteria good for gut health and immune health.
The human gastrointestinal tract is a complex and dynamic ecosystem referred to as the gut microbiota. It contains in average 100 trillion of symbiotic microorganisms, and features over 5,000 bacterial species.1
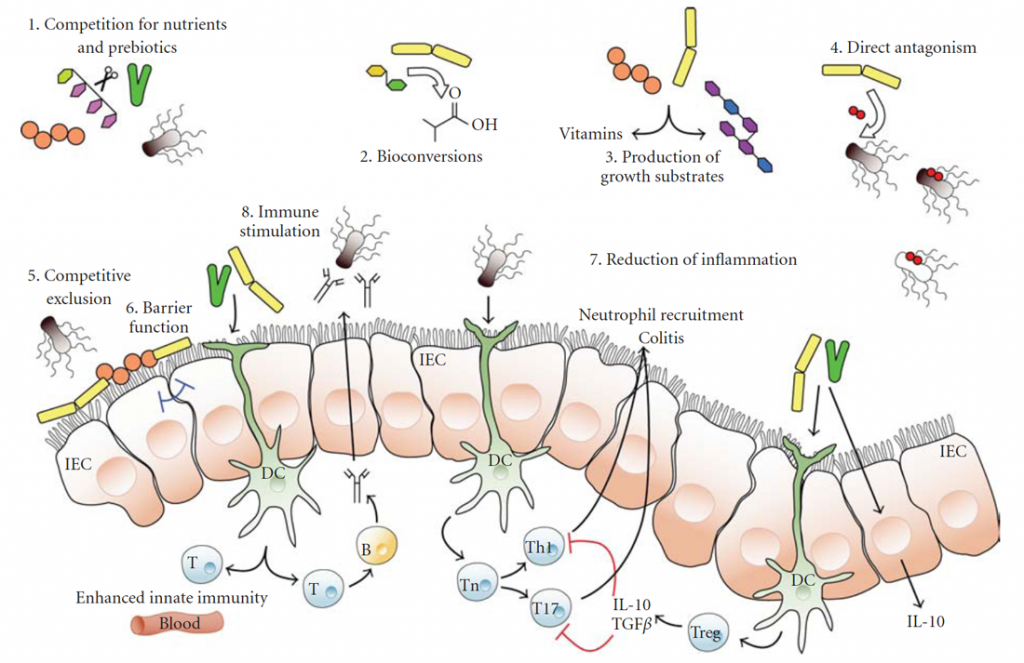
Many of these bacteria are beneficial and play significant roles in human health2 among others:
- Improve gut barrier function;
- Compete with pathogenic microbiota for nutrients, and adhesion to the gut and improve colonization;
- Stimulate, modulate and regulate host’s immune response (immunomodulatory);
- Regulate acute and chronic inflammation in intestinal mucosal tissue (anti-inflammatory properties) such as those with inflammatory bowel disease;
- Help physiological and metabolic functions;
- Modulate gastrointestinal hormone release and regulate brain behavior (gut-brain axis).
Probiotics have demonstrated beneficial effects on variety of gastrointestinal diseases3 such as:
- Acute infectious diarrhea
- Antibiotic-associated diarrhea
- Constipation
- Functional gastrointestinal disorder
- Irritable bowel syndrome (IBS)
- Necrotizing enterocolitis
- Ulcerative colitis
In most cases, probiotics mainly strains of Lactobacillus or Bifidobacterium species, come from the gut microbiota of healthy humans, plants and dairy products. It also happens these are the two most studied, and widely used probiotic genera. Lactobacillus and Bifidobacterium are the only probiotic genera classified under the US FDA GRAS (Generally Regarded As Safe) designation.
Postbiotics are metabolic by-products produced by probiotics during fermentation, and posses similar protective roles and health promoting effects as probiotics.
Postbiotics have no live bacteria.
These bioactive compounds are able to exert beneficial health effects, among others:
- Improve gut barrier function;
- Compete with pathogenic microbiota for adhesion sites at gastrointestinal level;
- Protect against pathogens;
- Re-establish balanced microbiota composition and healthy native microbiota;
- Stimulate, modulate and regulate host’s immune response (immunomodulatory);
- Posses anti-inflammatory, antioxidant, anti-infectious activities;
- Help physiological and metabolic functions.
Clinical studies have indicated postbiotics exert beneficial effects4,5,6, on gastrointestinal and extra-intestinal issues such as:
- Bloating
- Constipation
- Diarrhea
- Gastroesophageal-Reflux Disease (GERD)
- Irritable Bowel Syndrome (IBS)
- Crohn’s Disease
- Ulcerative Colitis
- Type 2 Diabetes
- Kidney Disease
- Atopic Dermatitis
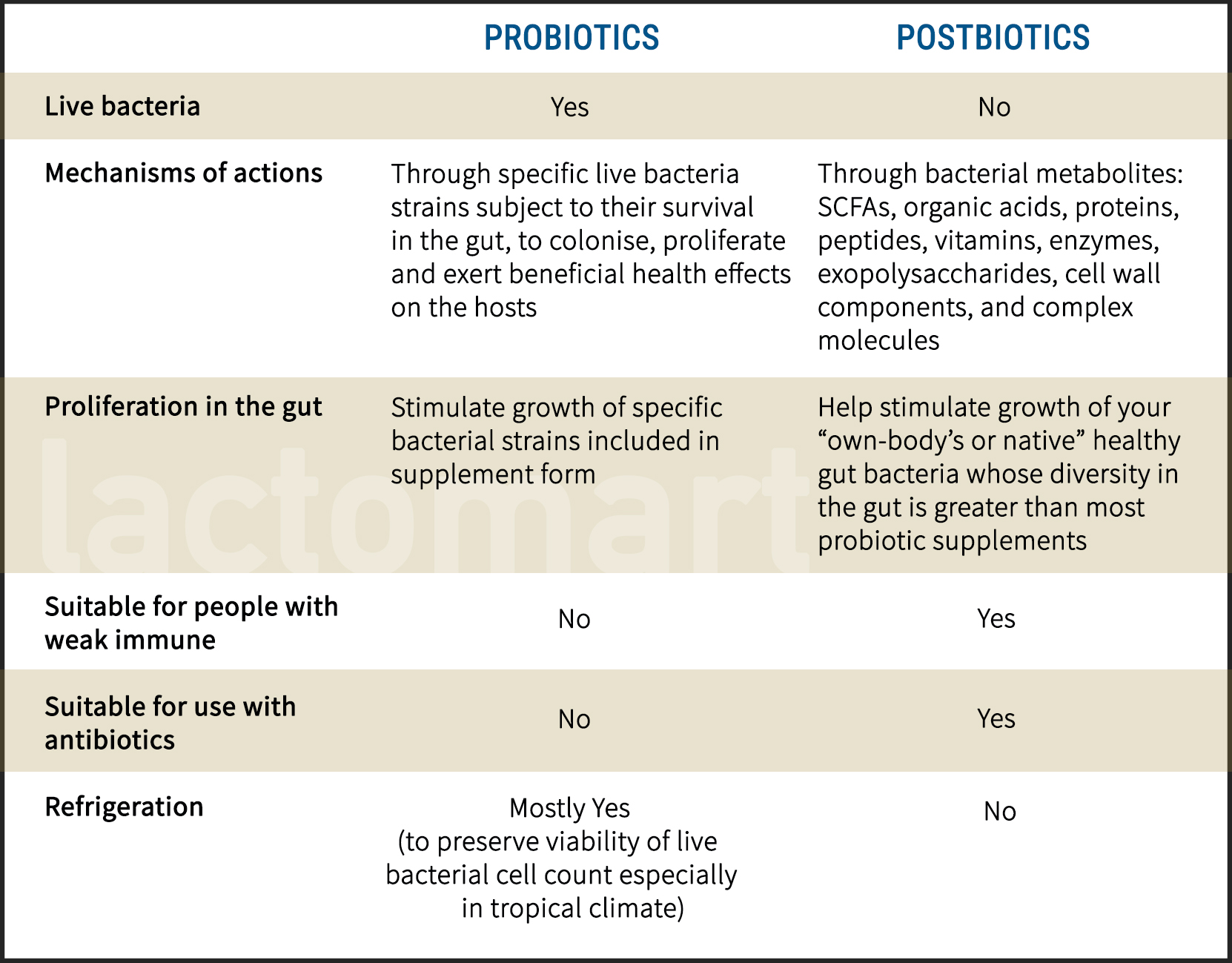
While probiotics efficacy depends on live bacteria and subject to their survival in the gut, postbiotics efficacy is based on microbial metabolites: short-chain fatty acids (SCFAs), organic acids, functional proteins like bacteriocins, peptides, vitamins, exopolysaccharides, enzymes, cell wall components or other complex molecules generated during fermentation.7
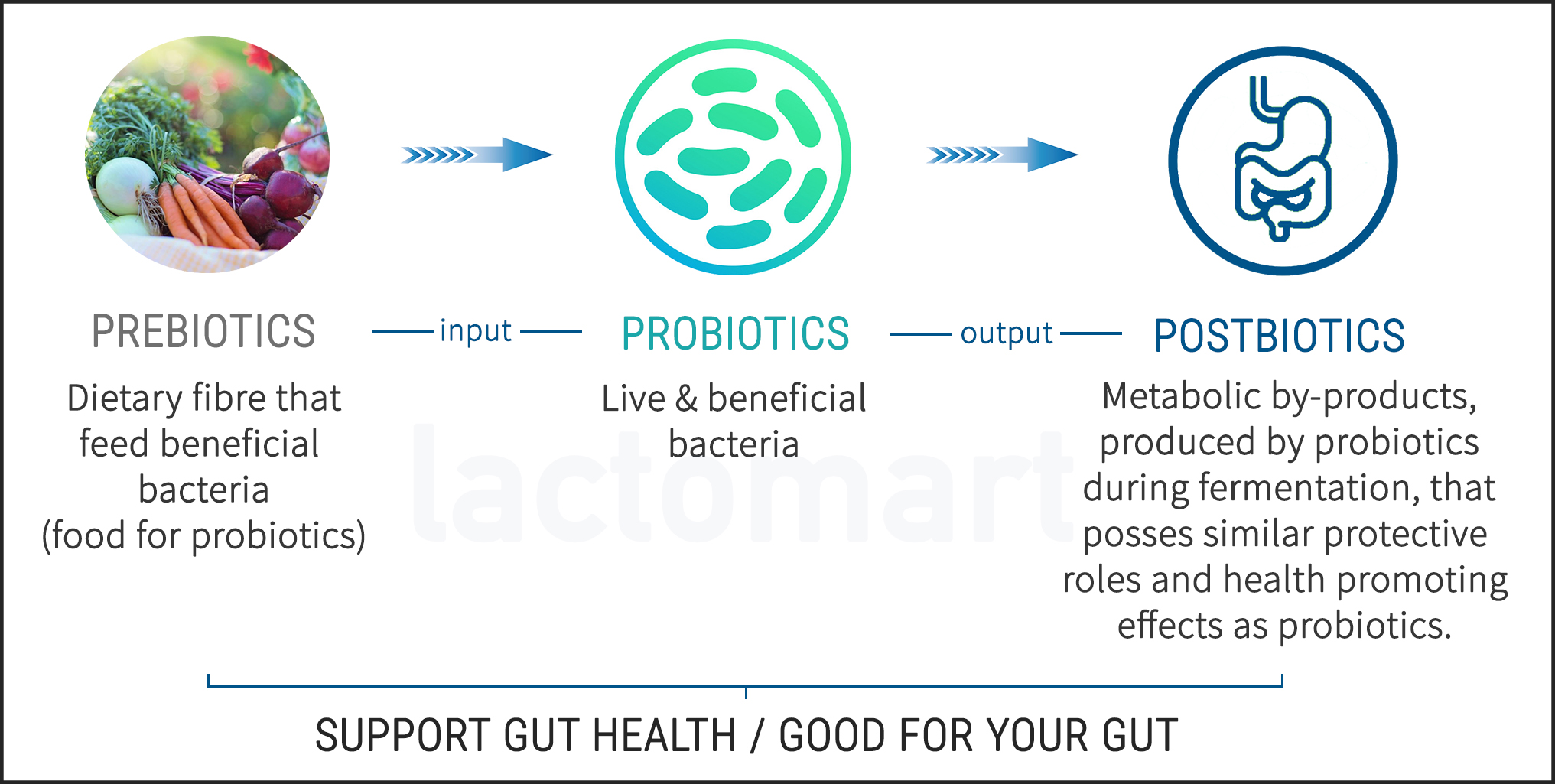
Probiotics and postbiotics work on different mechanisms of actions, and both are beneficial on gut health.
A healthy gut allows your body to absorb essential nutrients more efficiently and builds a strong immune system, naturally.
The questions most commonly asked is “Since both are good so which one do I take or which one is better?”
The answer is take both, together or interchangeably, for comprehensive benefits. Otherwise either one that you can get a hold of.
With the exception of consumption by immune-compromised individuals, adjunct use with antibiotics, and frequent travelers. This is where postbiotics make an excellent choice for these group of individuals.
Studies indicated both probiotics and postbiotics exert beneficial effects in management of irritable bowel syndrome (IBS).8
Interestingly, early studies indicated postbiotics administration has shown more favourable effects than probiotics as therapeutic aids in inflammatory bowel diseases (IBD) namely Crohn’s disease and ulcerative colitis9
- Aline Corado Gomes, Allain Amador Bueno, Rávila Graziany Machado de Souza and João Felipe Mota: Gut microbiota, probiotics and diabetes. Gomes et al. Nutrition Journal 2014, 13:60.
- Rout George Kerry, Jayanta Kumar Patra, Sushanto Gouda, Yooheon Park, Han-Seung Shin, Gitishree Das: Benefaction of probiotics for human health: A review. Journal of food and drug analysis 26 (2018) 927 e9 39.
- Thad Wilkins, Jacqueline Sequoia: Probiotics for Gastrointestinal Conditions: A Summary of the Evidence. Am. Fam. Physician 2017, 96, 170–178.
- Núria Piqué , Mercedes Berlanga and David Miñana-Galbis: Health Benefits of Heat-Killed (Tyndallized) Probiotics: An Overview. Int. J. Mol. Sci. 2019, 20, 2534.
- Tomonori Sugawara, Daisuke Sawada, Yu Ishida, Kotaro Aihara, Yumeko Aoki, Isao Takehara, Kazuhiko Takano & Shigeru Fujiwara: Regulatory effect of paraprobiotic Lactobacillus gasseri CP2305 on gut environment and function. Microbial Ecology in Health and Disease, 27:1, 30259.
- Yasuhiko Komatsu, Tomoya Sasaki, Masami Ohishi: Effect of Heat-Killed Lactobacillus johnsonii No. 1088 on Gastroesophageal Reflux Disease-Related Symptoms: A Pilot Clinical Study. American Journal of Food Science and Health Vol. 2, No. 6, 2016, pp. 176-185.
- Carrie A. M. Wegh, Sharon Y. Geerlings, Jan Knol, Guus Roeselers and Clara Belzer: A Review: Postbiotics and Their Potential Applications in Early Life Nutrition and Beyond. Int. J. Mol. Sci. 2019, 20(19), 4673.
- Debora Compare, Alba Rocco, Pietro Coccoli, Debora Angrisani, Costantino Sgamato, Barbara Iovine, Umberto Salvatore and Gerardo Nardone: Lactobacillus casei DG and its postbiotic reduce the inflammatory mucosal response: an ex-vivo organ culture model of postinfectious irritable bowel syndrome. Compare et al. BMC Gastroenterology (2017) 17:53.
- Katerina Tsilingiri, Theolis Barbosa, Giuseppe Penna, Flavio Caprioli, Angelica Sonzogni, Giuseppe Viale, Maria Rescigno: Probiotic and postbiotic activity in health and disease: comparison on a novel polarised ex-vivo organ culture model. Gut 2012;61:1007e1015.
Related Products
Tags or keywords:
food poisoning | diarrhea | diabetes | gut health | immune health | nutrients | SCFA | prebiotics | probiotics | postbiotics | supplements | Lactobacillus | Bifidobacterium | gastrointestinal | vitamins | supplements | fermentation | metabolites | constipation | irritable bowel syndrome | IBS | IBD | inflammatory bowel diseases | ulcerative colitis | heat-killed probiotics | Crohn’s disease | immune-compromised | travel friendly | antioxidants | anti-inflammatory | bloating | eczema | kidney disease | GERD | acid reflux | heartburn | strong immune

